रोगास्तस्यापहर्तारः श्रेयशो जीवितस्य च।। - (Charaka Samhita)
[The foundation for performing Dharma, Artha, Kama and attaining Moksha is good health (Arogya). Diseases destroy that very foundation.]
Background
The healthcare sector is crucial to a country's overall well-being. As India has grown to become the world's most populous country, delivering adequate healthcare to all segments of society has emerged as a top priority. Good health and well-being are also Goal 3 of the United Nations' Sustainable Development Goals, which India aims to attain by 2030. India also seeks to fulfill its objective of Universal Health Coverage (UHC) by 2030. UHC assures that everyone has access to quality health care without incurring financial hardship.
Various constitutional provisions emphasize the importance of the right to health. Articles 38, 41, 42, and 47 of the Indian constitution direct the government to formulate policies regarding the health and well-being of the population. The Apex Court of India has also observed many times that the Right to Health is fundamental to the Right to Life (Article 21) as in the Paschim Banga Khet Mazoor Samity vs State of West Bengal (1996) case. In this case, the Supreme Court of India held that it is the responsibility of the government to provide adequate medical aid to every person and strive for the welfare of the public at large. [1]
Against this backdrop, public health, which includes promoting healthy behaviours, putting in place evidence-based measures, and assuring community well-being, has grown in importance. Rather than only treating individuals, public health aims to safeguard and improve the health of the entire population. It focuses on illness prevention, encouraging healthy practices, and creating circumstances in which everyone may have a healthy life. Beyond individual therapy, public health may also encompass environmental health. Taking all of this into account, one could argue that public health protection policies should be accessible across the country, from the busy streets of a major metropolis to remote settlements tucked away in the Himalayas.
However, there is a great disparity in spending on healthcare across the globe. As of 2020, the USA spends 18.86 percent in terms of GDP on Health, China spends 5.56 percent, Australia spends 10.65% while India spends only 2.96% on Health, which is one of the lowest in the World.[2] Additionally, public hospitals in India have not been in great shape. Public hospitals confront significant challenges such as inadequate infrastructure, insufficient staff, unmanageable patient loads, inconsistent service quality, and excessive out-of-pocket costs.[3] This has pushed economically weaker sections of the population to get their treatment in private hospitals, which makes expenditure on health one of the major out-of-pocket expenditures in India. This leads millions to fall below the poverty line every year, and the situation has aggravated with the COVID-19 pandemic.
In this aspect, the launch of the Ayushman Bharat initiative has been extremely beneficial, and the progress that has been gained so far is impressive. This article will focus on the accomplishments of the Ayushman Bharat programme as well as the challenges it faces. From there, some recommendations for improving its usefulness will be suggested.
Development of India’s Healthcare System and the Role of Ayushman Bharat
When India gained independence, the health infrastructure was in despair. The life expectancy was approximately 32 years, infant mortality rates were high, starvation was common, and infectious illnesses such as malaria, tuberculosis, and smallpox were prevalent. Over the course of its 75-year history, India's healthcare system has experienced both significant advancements and enduring difficulties. The initial decades were devoted to developing healthcare infrastructure and starting countrywide immunization programmes. It was on 23rd April 1977 that India eradicated smallpox through a major vaccination effort and elimination of smallpox was a big success and inspiration for those working in the Public Health sector.
Following the elimination of smallpox in 1977, India developed its first national health policy in 1983, with the objective of achieving "Health for All" by 2000. The programme concentrated on health infrastructure, building a network of Community Health Centres (CHCs) and Sub Health Centres (SHCs). This was followed by two revisions: 2002 and 2017. The National Health Policy of 2002 underscored the significance of ensuring more equitable access to health care across the country's socioeconomic and geographical boundaries. The emphasis has been on increasing overall public health investment through a significantly enhanced commitment from the Central Government. However, there were substantial gaps in the health plan, demanding a more comprehensive and innovative health strategy that would meet the demands of the health protection of the underprivileged.
A new national health Policy was formulated in 2017. The National Health Policy, 2017 defines its goal, “The policy envisages as its goal the attainment of the highest possible level of health and wellbeing for all at all ages, through a preventive and promotive health care orientation in all developmental policies, and universal access to good quality health care services without anyone having to face financial hardship as a consequence. This would be achieved through increasing access, improving quality and lowering the cost of healthcare delivery.” [4] Keeping this in mind, the Indian government launched its flagship scheme 'Ayushman Bharat'. Launched in 2018, as recommended by the National Health Policy, 2017 to achieve the goal of Universal Health Coverage (UHC). Ayushman Bharat is a major step taken by the Indian Government towards inclusive Healthcare. Ayushman Bharat has 2 major components- 1. AB-HWC (Ayushman Bharat-Health and Wellness Center) and 2. PM-JAY (Pradhan Mantri Jan Arogya Yojana). The scheme has 2 components which are complementary to each other. The first component targets Primary healthcare, while the second targets Secondary and Tertiary Healthcare.
PM-HWC
The key objective of establishing PM-HWC is to expand the range of health services provided at the primary level; a shift from selective primary healthcare to comprehensive primary healthcare. Under this component, the goal was to set up 1,50,000 Health and wellness centres, known as Ayushman Arogya Mandir and as of January 2024, more than 1,60,000 has been set up in the country. Through Ayushman Arogya Mandir the attempt is to deliver a comprehensive range of services spanning preventive, promotive, curative, rehabilitative, and palliative care.
PM-JAY
Pradhan Mantri Jan Aarogya Yojana, which is the second component of Ayushman Bharat, targets secondary and tertiary Healthcare. Under this, insurance cover of up to rupees 5 lakh is given to the beneficiary families. There are certain criteria for both rural and urban areas to avail the benefits of PM-JAY. For rural families, there are 6 deprivation criteria such as landless households, disability, no earning adult member and families belonging to the Scheduled Caste (SC) and Scheduled Tribes (ST) categories, etc. There are certain listed occupational categories (street vendors, domestic workers, manual labourers, etc.) as a criterion for an urban household to avail of the benefits of PM-JAY.
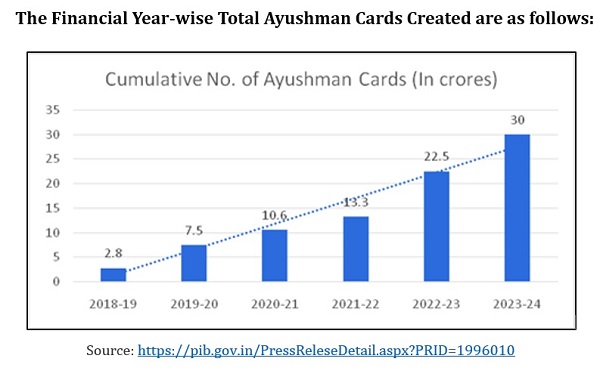
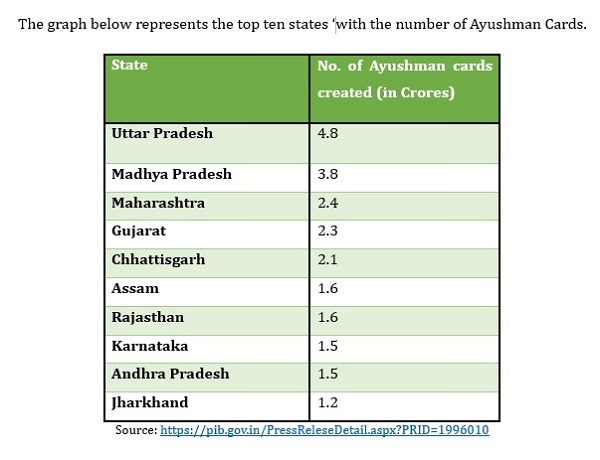
As mentioned earlier, this program is very diverse and extensive in its coverage if it is compared with the earlier schemes. PM-JAY has subsumed Rashtriya Swasthya Bima Yojana (RSBY) which was launched in 2008 by the UPA Government. Under RSBY, insurance coverage up to only 30,000 was given, it only covered secondary healthcare, and RSBY also had much lesser coverage than PM-JAY. RSBY covered only unorganized sector workers belonging to the BPL category and their family members and also had a cap of five members, under this the beneficiaries were roughly around 36 million families. While PM-JAY covers around 40% of the population of the country and the beneficiaries are chosen based on SECC (Socio-Economic Caste Census), as of January 2024, more than 30 crore Ayushman cards have been issued; Uttar Pradesh is the state with the highest number of Ayushman Bharat cards.[5]
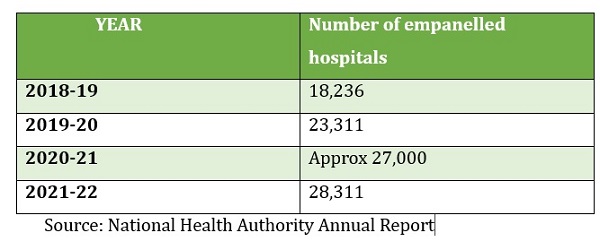
PM-JAY is fully funded by the government and the premium is shared between the Centre and the State on a 60:40 (Center: State) basis. In the North-eastern and the Hilly states, the funding is on a 90:10 (Center: State) basis. Under this scheme, both Private and Public hospitals are covered. As per the Annual Report 2021-22 by NHA, there are approximately 28,300 empanelled hospitals under this scheme out of which 46% are private and 54% are public hospitals.[6] The table below shows the number of empanelled hospitals under the scheme.
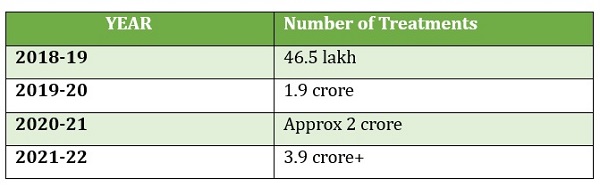
Within the 4 four years of its launch that is from 2018-19 to 2021-22, more than 3.9 crore+ treatments have been recorded under the scheme, amounting to 45,294 crore rupees out of which 4.9 crore treatments are inter-state, amounting to 1110 crore rupees. [7] The table below shows the number of treatments done under this scheme from 2018 to 2022.
Implementation
The scheme comes under the Ministry of Health and Family Welfare. It is implemented in 3 tiers. The National Health Authority (NHA) is responsible for the implementation of the scheme at the Central level. At the state level, the State Health Authority (SHA) is responsible for its implementation. The programme also has District Implementation Units (DIU).[8] The Governing Board of NHA comprises a chairperson and 11 members. Union Minister for Health and Family Welfare is the chairman of the Governing Body. It is headed by a full-time CEO supported by a Deputy CEO and Executive officers. From 2018-19, the organization was under the control of the Ministry of Health and Family Welfare, but after 2019, the organization became independent and accountable to its own board of experts and policymakers.[9]
There are 3 models in which the scheme is implemented by the states, which are Trust, Insurance, and Hybrid models. Under the Trust model, claims are paid directly by the SHAs, under the Insurance model, claims are paid by the Insurance company, and the SHA pays a premium to the insurance company and under the Hybrid model, claims up to a certain amount of cover are paid by the insurance company and claims over and above this amount are paid by SHAs directly.[10]
Because of the efficiency of the implementation of the Ayushman Bharat programme, it has turned out to be a successful scheme. It has also contributed to the advancement of the public health infrastructure and Health protection of the economically weaker section of the Society. With the Union Budget announcement for 2024-25, its coverage has been further expanded which will also require a piece of updated machinery to implement it efficiently.
Challenges
While the scheme performs effectively and provides social security to the underprivileged citizens of society, it has frequently been distorted by politics. One of the main issues faced by the scheme is because of Center-State politics. Under the Seventh Schedule of the Constitution of India, Public Health and Sanitation is a State subject which means that it is up to the discretion of the State Government if they want to adopt the scheme made by the Center on Public Health. The scheme is not implemented by West Bengal, Orissa, and Delhi.[11] As of the 2011 census, combining the population of West Bengal, Orissa, and Delhi, is approximately 13 crore which means that the huge population of the country suffers because of the disagreements between the Center and the States.
Instead of accepting PM-JAY, these states run their health protection schemes that offer similar benefits like Swasthya Sathi of West Bengal and Biju Swasthya Kalyan Yojana of Orissa, both of these schemes offer insurance claims up to 5 lakh which is similar to PM-JAY, but the problem with this is that it puts a lot of on the State's exchequer as there is no sharing between States and the Center, here whole financial burden is borne by the State and if they had implemented PM-JAY, they could have made available the same benefits to their population by giving on 40% of the amount of premium. Other than adoption, the problem that arises because of politics is in the implementation. Even the States with different party governments as of Center which have adopted the scheme have not been performing very well, Kerala being an exception. For instance, the percentage of claims paid by Rajasthan is only 2.5% and that of Telangana is only 25.6%.
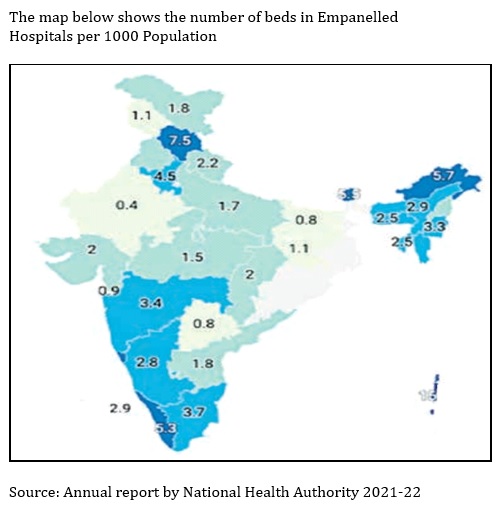
The lack of hospitals is another challenge faced by this scheme. Combining Public and Private hospitals, India has around 69,000 hospitals, of these 43,000 are private hospitals and 25,778 are public hospitals which means private hospitals account for 62% of India's Health Infrastructure (2019).[12] But as of 2022, only 28,311 hospitals got empanelled under PM-JAY and of these, only 46% are Private Hospitals, this means Private Hospitals are somewhat hesitant. Another issue is of low availability of beds in the empanelled hospitals under PM-JAY.
Other major problems for AB include inadequate understanding of PM-JAY, difficulty in comprehending complicated products like as health insurance by the poor, and the complexity of creating Ayushman Cards.
Way Forward
While the scheme is a great step taken by the Indian government towards inclusive healthcare, there is a need to remove the obstacles coming in its way to make it an even bigger success. The Center and States should work on the principle of cooperative federalism. The centre and the states should work together for the better implementation of this scheme. The states that have not adopted this scheme should be convinced to adopt this as this can help them to save a lot of money and with that money, they can focus on other issues like poverty. We need to take more and more private hospitals in our confidence to get empanelled under this scheme as the contribution from the private sector can help a lot.
Increasing the Public Health Infrastructure is also necessary to improve the usefulness of this programme. As previously said, there is an acute problem with the number of beds per individual and it needs to be addressed. Health and wellness are given highest importance since they are essential parts of Ayushman Bharat. There is a pressing need to strike a balance between the increased emphasis on health and a falling emphasis on wellness. This programme will also be more profitable if it raises its awareness and streamlines the enrolment procedure.
Conclusion
India's economy is currently the fifth largest in the world, with goals to rise to the third rank by 2025. Also, we have surpassed China as the world's most populous country. These two factors are critical and have a direct impact on healthcare. A country cannot prosper unless its population is in good health. Programmes such as Ayushman Bharat, which guarantee health protection for the marginalized segment of society, play a crucial part in the development of the nation and help manage the healthcare system of the most populous country in the world. The Ayushman Bharat has so far produced excellent results, but in order to achieve even greater results, it will need to be updated periodically and implemented throughout the nation with effective mechanisms.
References
[1] ‘Right to Health as a Fundamental Right Guarenteed by the Constitution of India’, jsalaw, March 22, 2020. https://www.jsalaw.com/covid-19/right-to-health-as-a-fundamental-right-guaranteed-by-the-constitution-of-india/#:~:text=Union%20of%20India%20AIR%201995,fundamental%20right%20under%20Article%2021.
[2]https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?locations=IN&view=map
[3] Vikas Bajpai, "The Challenges Confronting Public Hospitals in India, Their Origins, and Possible Solutions", Advances in Public Health, vol. 2014, Article ID 898502, 27 pages, 2014. https://www.hindawi.com/journals/aph/2014/898502/
[4] National Health Policy, 2017. https://main.mohfw.gov.in/sites/default/files/9147562941489753121.pdf
[5] ‘30 crore Ayushman Cards created under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana’ PIB Releases, January, 14, 2024. https://pib.gov.in/PressReleseDetail.aspx?PRID=1996010
[6]National Health Authority, Annual report, 2021-22. https://nha.gov.in/img/resources/Annual-Report-2021-22.pdf
[7] Ibid.
[8] Ibid.
[9] https://nha.gov.in/NHA
[10]National Health Authority, Annual report, 2021-22. https://nha.gov.in/img/resources/Annual-Report-2021-22.pdf
[11] Health Ministry urges Delhi, Odisha, West Bengal to join AB-PMJAY scheme, The Hindu, September 25, 2023. https://www.thehindu.com/news/national/health-ministry-urges-delhi-odisha-west-bengal-to-join-ab-pmjay-scheme/article67344896.ece
[12] Estimated number of public and private hospitals across India in 2019. https://www.statista.com/statistics/1128425/india-number-of-public-and-private-hospitals-estimated/#:~:text=An%20estimated%2069%20thousand%20public,number%20of%20hospitals%20that%20year.
(The paper is the author’s individual scholastic articulation. The author certifies that the article/paper is original in content, unpublished and it has not been submitted for publication/web upload elsewhere, and that the facts and figures quoted are duly referenced, as needed, and are believed to be correct). (The paper does not necessarily represent the organisational stance... More >>
Image Source: https://www.probusinsurance.com/wp-content/uploads/2023/04/Ayushman-Bharat-Yojana-PMJAY.jpg










Post new comment